News
Glaucoma
What is Glaucoma?
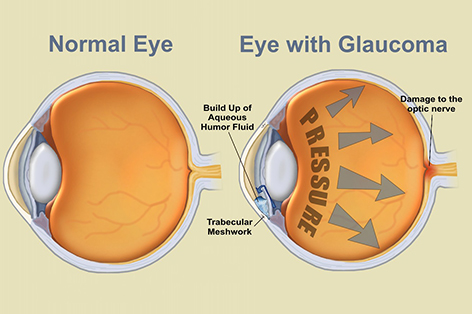
Glaucoma is a progressive eye disease caused by increase in fluid pressure of the eye that results in damage to the optic nerve. Because the optic nerve transmits the visual information from the eyes to the brain, glaucoma can result in vision loss and blindness. However, with early detection and treatment, you can often protect your eyes against serious vision.
What causes glaucoma?
Glaucoma is most often caused by abnormally high pressure inside the eye caused by buildup of aqueous humor, a clear fluid which is constantly produced inside the eye. The fluid buildup happens when the channels draining the fluid out of the eye are defective (open angle) or obstructed (closed angle), thus leading to rise in eye pressure and optic nerve damage.
What are the symptoms of Glaucoma
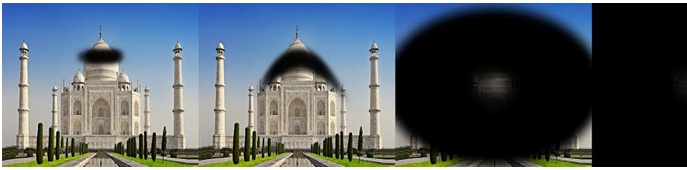
Glaucoma has been called the silent thief of sight as there may not be any symptoms until the disease reaches an advanced stage. In the more common open angle type, the eye pressure builds up slowly causing gradually progressive optic nerve damage. Patients slowly lose their peripheral (side) vision until they seem to be looking through a tunnel. Over time, central vision may worsen until no vision finally remains.
The closed angle type may present with sudden rise in eye pressure causing headache, eye pain, redness, decreased vision, rainbow halos around lights and may be associated with systemic symptoms like nausea and vomiting.
What are the risk factors for glaucoma?
Factors which increase the risk of having glaucoma are high intraocular pressure , older age (>40 years), race (Africans, Hispanics have higher incidence of open angle glaucoma, Asians have more closed angle type), positive family history, systemic diseases (diabetes, hypertension, thyroid), use of longterm steroid medications, nearsightedness (myopia), eyeball injuries etc.
FAQ's
How is glaucoma diagnosed?
Anyone having the above mentioned risk factors should undergo comprehensive eye checkup to detect glaucoma. At Winvision, we have a state of the art glaucoma clinic which provides the following facilities for glaucoma diagnosis:
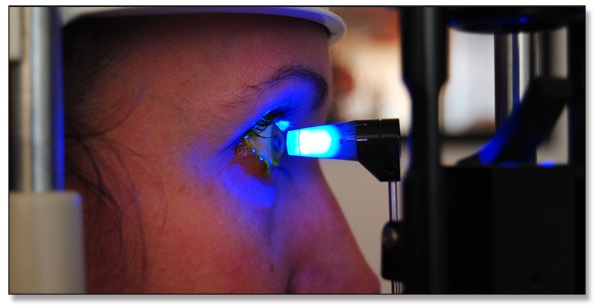
- Tonometry: This measures the pressure within your eye by applying pressure to the cornea with a tiny device (applanation tonometer) or a puff of air (noncontact tonometer). Normal intraocular pressure (IOP) is generally between 12-22 millimeters of mercury.
 .
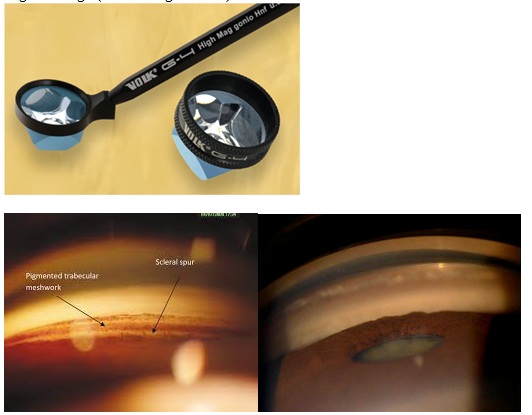
. - Gonioscopy: This is done to visualize the drainage passage of the eye called the angle which is the junction between the iris and the cornea. A handheld device called gonioscope is placed on the cornea to assess whether the angle is open or closed. In addition, other causes of secondary glaucoma like new blood vessels (neovascular glaucoma) , abnormal angle anatomy (congenital or glaucoma by birth), angle damage (traumatic glaucoma) can be identified.
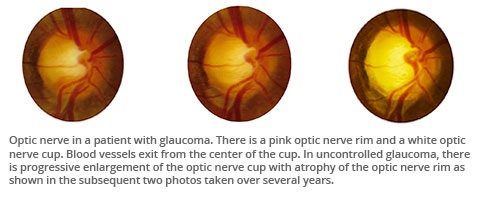
- Ophthalmoscopy: This is a test where the doctor looks at the inside of the eye and retina by using a special light and magnifying lenses to see if there are any signs of damage to your optic nerve.
- Pachymetry: This is used to measure the central corneal thickness (CCT) which influences the accuracy of the tonometry readings. Unusually thin or thick corneas can under or overestimate the eye pressure values. Research suggests patients with thin corneas are three times more likely to develop glaucoma.

- Fundus photography: Serial photographs of the optic nerve head allows the practitioner to evaluate fine details of the anatomy not easily seen on examination. In addition, photographs allow for analysis of changes in the anatomy of the optic nerve over time. It is also less expensive compared to other imaging modalities.

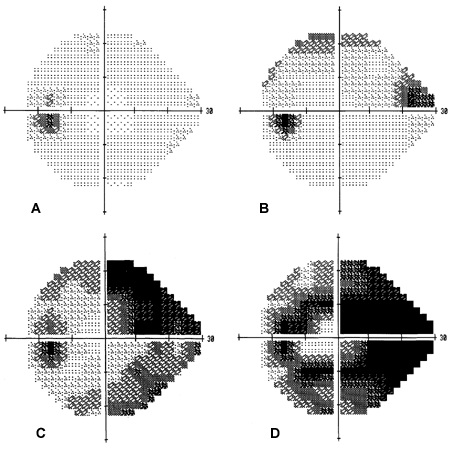
- Perimetry (Visual fields): The Humphrey Field Analyzer measures the peripheral vision. The patient sits in front of a bowl shaped machine and stares at a central spot of light. Tiny spots of light of varying intensity are randomly projected inside the bowl and a button is pressed as soon as a light is seen. A computer printout shows the seen and non-seen areas and also indicates the intensity of light visualized.

- Optical coherence tomography: This is a non-contact, noninvasive imaging technique which demonstrates the structure of the optic nerve head, retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC) by analyzing the interference patterns of reflected laser light. It is well known that structural RNFL loss precedes the onset of visual field defects, thus OCT is especially useful in helping to diagnose early glaucoma not yet detectable by perimetry.

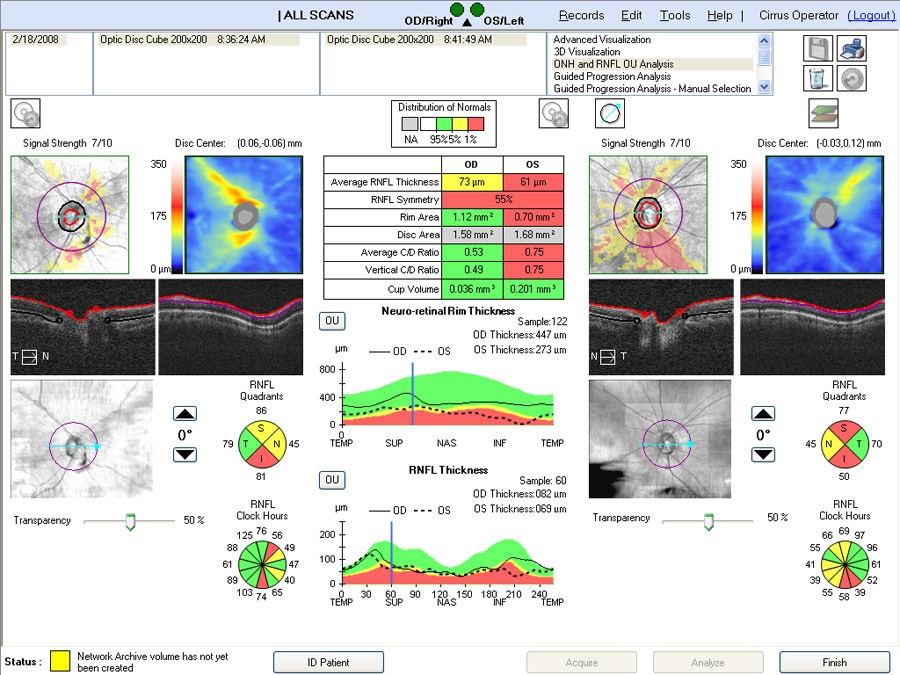
The ZEISS glaucoma suite at Winvision comprises essential diagnostic technologies such as Cirrus™ HD-OCT, a full spectrum powerhouse OCT with expanded glaucoma applications, Humphrey®Field Analyzer 3(HFA™), a premier automated visual field analyzer considered a gold standard in glaucoma care and the new VISUCAM® 524 fundus camera with the 24 megapixel sensor which provide superior clarity and ultra high resolution fundus imaging.
How do you treat Glaucoma?
Reducing eye pressure is the only way to save vision loss due to glaucoma. Treatment depends on the type of glaucoma-mild, moderate, or advanced and may involve prescription medications- usually eye drops or surgery or both.
Eye Drops
They work by helping fluid drain better or by decreasing the amount of fluid made by the eye, and some do both. Your doctor may prescribe a single type of eye drops or a combination of types. You may need more than one medication to keep your eye pressure low enough. Some important tips to follow while using drops:
- Be sure to use eye drops every day, exactly as instructed and if possible, at the same time everyday.
- Some medications may cause side effects like redness, itching, headache. Please report to your doctor but never discontinue the drug unless advised.
- Use the bottle within one month of opening and store it in a cool dark place preferably in a refrigerator.
- It is important to have periodic eye pressure checkup to ensure that the condition is stable. Your doctor may advise annual perimetry or OCT to confirm these changes.
- Please understand that glaucoma is a chronic disease, so eye drops may be needed even lifelong. Discuss any problems including cost with your doctor. The low cost generic drugs work as effectively as the branded ones.
Surgery
If eye drops do not lower intraocular pressure enough, your doctor may prescribe surgery. Surgery cannot reverse vision loss, but it can help lower eye pressure by improving the flow of fluid out of the eye. But this doesn't necessarily mean you won't have to take eye drops any more, and surgery may need to be repeated. Indications of surgery are.
- To stabilize very advanced disease by reducing pressure fluctuations
- Presence of other comorbidities like cataract
- Intolerable side effects to medications
- Patient unable to use drops as advised (poor compliance)
There are two main types of surgery: laser and conventional.
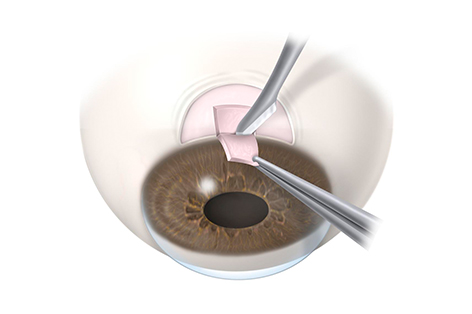
Laser surgery involves application of a small beam of light to the eye's drainage system to help fluid flow out of the eye. When laser surgery does not lower eye pressure enough, or the pressure starts to rise again, the doctor may recommend conventional surgery. Conventional surgery (trabeculectomy) or filtration surgery is indicated after failed medical therapy and laser surgery. A new drainage passage is created in the white part of the eye called sclera through which the fluid can drain out and get absorbed into the blood vessels around the eye. Though trabeculectomy is the most commonly performed glaucoma surgery, certain alternatives are useful in selected cases. These include:
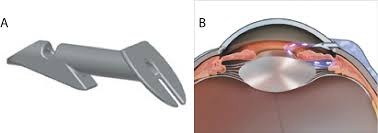
- Tube Shunts - small tubes made of silicone (Ahmed valve)or other materials are surgically inserted into the eye to provide an alternative pathway for fluid (aqueous) to drain.
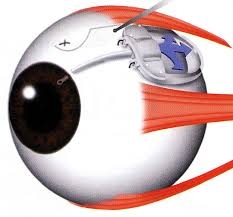
- Filtration device - An artificial drainage device made of stainless steel (Ex-Press shunt) is used to help drain fluid out of the eye.
What are the precautions one must follow after glaucoma surgery?
Recovery from trabeculectomy may take upto eight weeks. Frequent office visits may be needed, often weekly, to check eye pressure and make necessary adjustments to the bleb so that the pressure is not too high or too low. During this period, vision will be blurred and it is advisable not to let water in the eye for 2 weeks and avoid activities like reading fine print, driving, bending, lifting weights and performing certain yoga and breathing exercises. Like in any surgery there may be complications like too low pressure (hypotony), scarring and closure of the drainage passage leading to failure of the bleb, bleb leaks and rarely, bleeding or infection. If the IOP is high, doctor may prescribe additional glaucoma medications or repeat surgery. Whatever the outcome, close monitoring is required after surgery also.
Recent advances in glaucoma management
Research in glaucoma continues around the world encompassing every aspect of the disease, be it gene-based disease detection and treatment, developing newer drugs and surgical devices and newer treatment modalities. Stem cells are being investigated as a possible treatment for glaucoma because they may have the potential to protect the optic nerve from further damage and slow the progression of vision loss due to glaucoma.


