News
Vitreoretina and Uvea Services
The department deals with the management of diabetic retinopathy, retinal detachment, ARMD, infections, trauma & various other retinal disorders. An exclusive retinal examination may be different than a routine eye exam. It involves dilation of your pupils, examination by the specialist and diagnostic testing if required. It may take about three hours for the complete examination. If treatment is recommended for your condition, it my take a little more time to perform the procedure. Surgical intervention if required can be scheduled at an appropriate time, depending on your condition.
- Dilation enlarges your pupils to allow the doctor a better view inside your eye. It is important to know that your vision will be blurred and you will be sensitive to light for 3 to 4 hours following this. Therefore, we recommend that you do not not drive after your appointment.
- Most diagnostic tests that the doctor may order to evaluate your eye condition can be performed in the outpatient on the same day.
- Many of the procedures (treatments) that may be recommended to treat your condition can be performed by the doctor in the outpatient as well.
- We also have a well equipped operation theatre for vitreoretinal surgery.
Common OPD Procedures:
Fundus Photography
Color photographs of the back of the eyeFluorescein Angiography (FFA) -
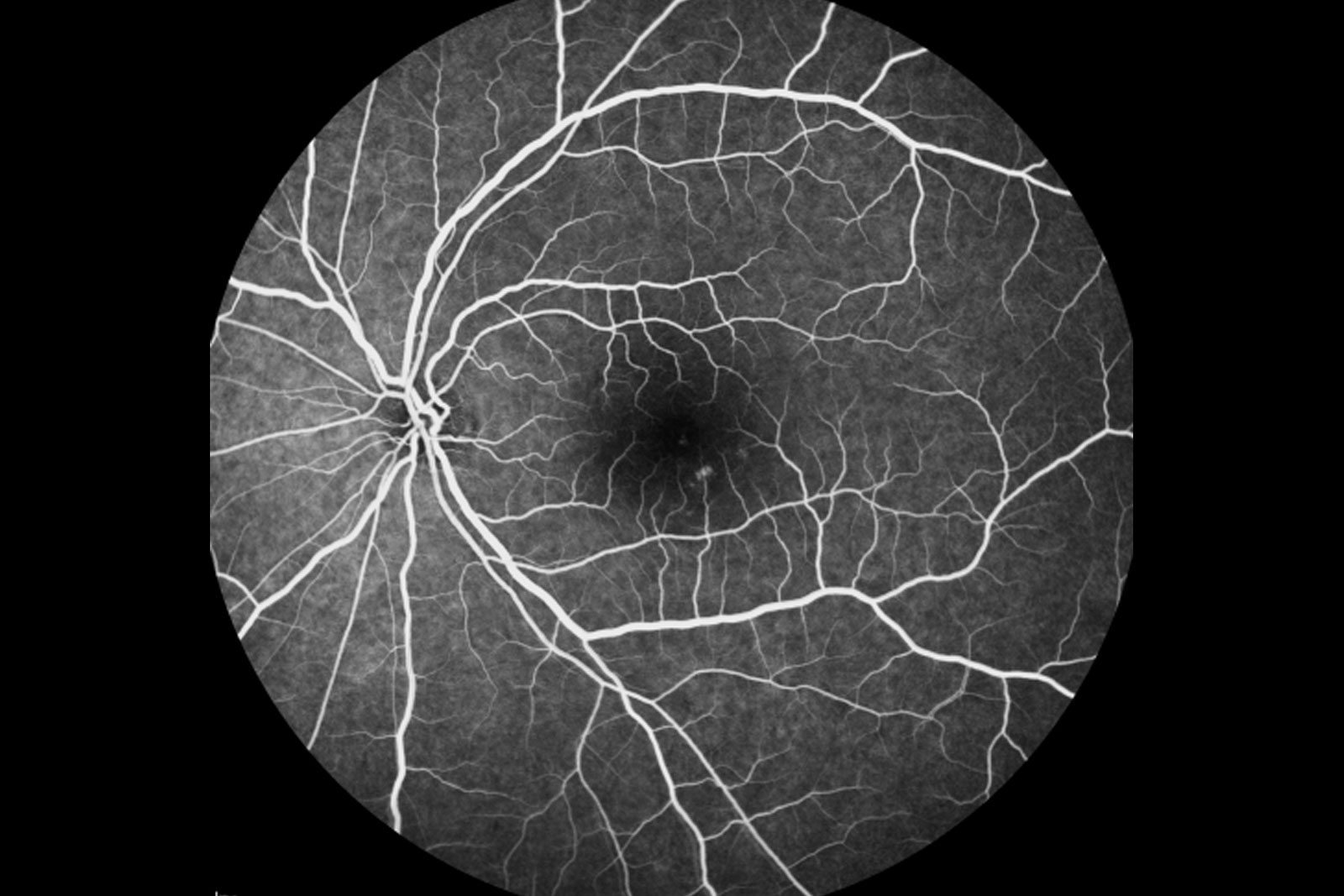

A diagnostic procedure that photographs the blood circulation of the retina. This involves injection of a dye called fluorescein into a vein in the arm or hand. It is recommended that the patients come fasting at least 2 hours prior to undergo the procedureIndocyanine Green Angiography (ICG) -Spectralis HRA system
A diagnostic procedure that photographs the blood circulation of the choroid. (Choroid is a layer of blood vessels behind the retina). This procedure is very similar to fluorescein angiography and involves injection of the indocyanine green dye into a vein in the arm or hand.Optical Coherence Tomography
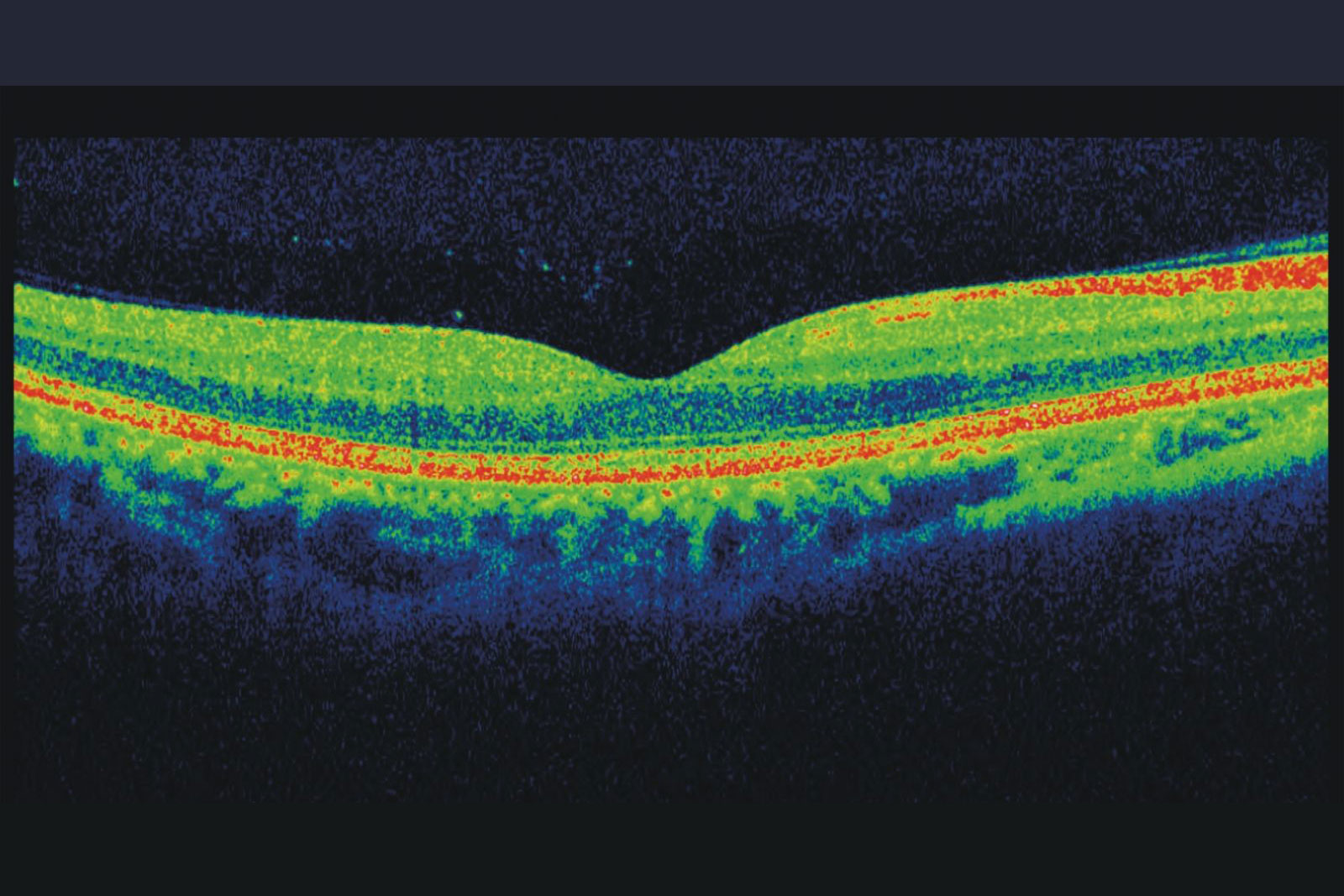

This is a diagnostic procedure similar to the CT scan of the brain. It uses a beam of light and its reflection to obtain cross-sectional images that provide information about the different layers of the retina. It is very useful to dignose macular edema( fluid collection in the maculr area due to various cause like diabetic retinopathy, Retinal Vein occlusions etc)Ultrasonography (B-Scan)

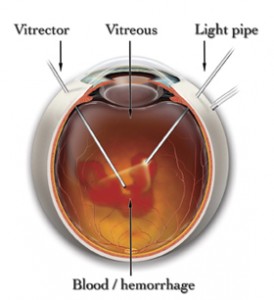
This procedure involves examining the eye when the normal view is obscured by hemorrhage(blood inside the eye) or cataracts.
Common Diagnostic Tests:
Lasers
 Indirect Ophthalmoscopic Laser Delivery System (LIO)
Indirect Ophthalmoscopic Laser Delivery System (LIO)This laser delivery system is mainly used for peripheral retinal lesions, e.g. horse shoe tear (HST), lattice degeneration, retinal holes, Retinopathy of prematurity (ROP) or pan retinal photocoagulation for vascular retinopathy in a hazymedia. It is also a very good tool to perform lasers for diabetic retinpathy.
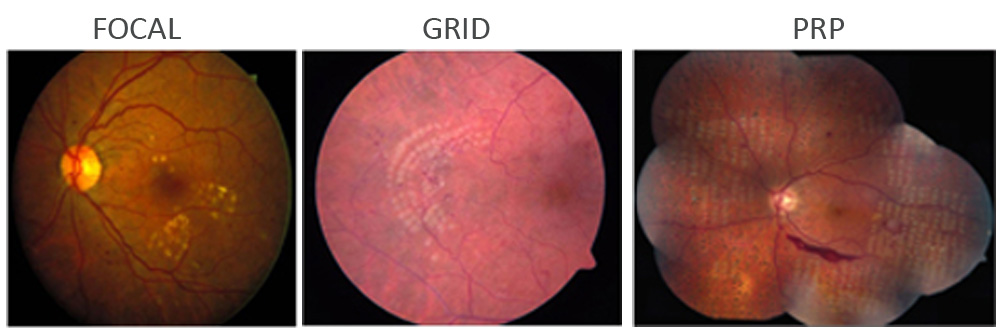
This is used to treat macula involved in diabetic retinopathy
CRYOTHERAPY
Cryotherapy is a second way of treating retinal tears apart from laser. An extremely cold probe is used to freeze a small area on the outside of the eyeball that overlies the retinal tears. The purpose is to seal the tears and create an eventual scar that will “stick” the retina to that spot.
Intra-Vitreal Injections
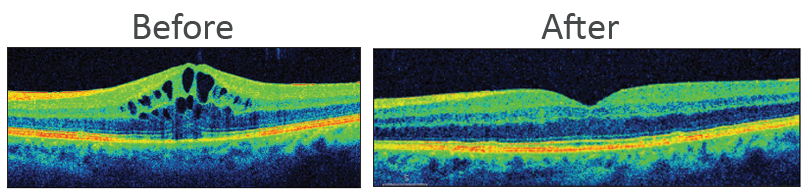
This is a procedure where a drug is injected into the vitreous cavity , which is the jelly-like substance inside your eye. It is performed to place medicines inside the eye near the retina.
Common conditions treated with intravitreal injections include diabetic retinopathy, macular degeneration, retinal vascular diseases and ocular inflammation.
The procedur is performed in operation room, It is done under aspepsis, , the actual procedure may take around 10 minutes . You will be made to lie down in a comfortable position and anaesthetic (numbing) drops will be applied in your eye. Your eye will be cleaned with an iodine antiseptic solution. A speculum is inserted and the medicine injected into the vitreous. You may experience a mild discomfort during the procedure. Antibiotic drops will be applied and the eye padded. Antibiotic eye drops need to be instilled for a week.
The doctor will see you the next day for inflammation or increase in intraocular pressure.
Instructions following an intravitreal injection
- There are no special precautions except to avoid rubbing the eye and washing your eye with water
- Instill the antibiotic eyedrops 4 times a day for 1 week.
- You can also take mild painkillers to alleviate any discomfort during the first few days.
Normal effects following an intravitreal injection
- A subconjunctival haemorrhage (red eye) usually occurs at the injection site. This will gradually fade within 7 to 10 days.
- Your vision may become slightly more blurred immediately after the injection. There may also be some floaters in your vision.
- You may experience mild discomfort for a few days after the injection. This discomfort should be relieved by mild painkillers.
Warning symptoms following an intravitreal injection
Although retinal detachment and cataract are potential but rare complications of intravitreal injection, the most feared complication is endophthalmitis i.e. infection inside the eye (rates typically less than 1%).
The warning symptoms of this complication are rapid onset of:
- Increasing eye pain.
- Increasing redness of the eye.
- Greatly decreased vision.
You must contact the hospital immediately for advice if you develop these warning symptoms. It is very important to identify and treat this type of infection as quickly as possible.
- Intravitreal Injections
- Various drugs used
- Accentrix
- Razumab
- Eylea
- Pagenax
- Ozurdex
- Triamcinolone
Conditions where Intra Vitreal injections are administered
- Diabetic Macular edema
- Clinically significant Macular Edema
- Edema due to Retinal Vein Occlusions
- Choroidal Neo Vascular Membrnes
- Endophthalmitis(Anti Biotics)
Retinal Detachment
retinal detachment is a separation of the retina from its attachments to the underlying tissue within the eye.
Most retinal detachments are a result of a retinal break, hole, or tear. Most retinal breaks, holes, or tears are not the result of trauma but are due to preexisting factors such as high levels of myopia, prior ocular surgery, and other eye diseases.
Flashing lights and floaters may be the initial symptoms of a retinal detachment or of a retinal tear that precedes the detachment itself.
Early diagnosis and repair of retinal detachments are important since visual improvement is much greater when the retina is repaired before the macula or central area is detached.
The surgical repair of a retinal detachment is usually successful in reattaching the retina.
What are retinal detachment symptoms and signs?
Flashes of light and floaters may be the initial symptoms of a retinal detachment or of a retinal tear that precedes the detachment itselfPeople with these symptoms should see an eye doctor and get his/her retinal examination. The symptoms of flashing lights and floaters may often be unassociated with a tear or detachment and can merely result from a separation of the vitreous gel from the retina.
Risk Factors
- Lattice Degeneration
- High Myopia
- Trauma
- Family History
Treatment Options
- Vitrectomy
- Scleral Buckling
- Cryotherapy
- Pneumatic Retinopexy
Surgery
Vitrectomy is a type of eye surgery that treats disorders of the retina and vitreous. The retina is the light-sensing tissue found lining the inside back part of the eye. Thevitreous is the clear, jelly-like substance that fills the inside of the eye. The vitreous is removed during vitrectomy surgery and usually replaced by a saline-type solution.
Why Vitrectomy
- Diabetic retinopathy, where there is bleeding and scar tissue
- Retinal detachments
- Wrinkling of the retina (macular pucker)
- Macular hole (partial loss of vision for fine details)
- Certain problems after cataract surgery
- Infection inside the eye
- Severe eye injury
Scleral Buckling Surgery for Retinal Detachment
Scleral buckling surgery is a common way to treat retinal detachment. It is a method of closing breaks and flattening the retina. A scleral buckle is a piece of silicone sponge, rubber, or semi-hard plastic that is placed on the outside of the eye (the sclera, or the white of the eye). The material is sewn to the eye to keep it in place. The buckling element is usually left in place permanently. The buckle does not prevent a retinal break from opening again. Usually extreme cold (cryopexy) or, less commonly, heat (diathermy) or light (laser photocoagulation) is used to scar the retina.
UVEA
Uvea is the middle part of the three coats of the eye. This further consists of the iris, ciliary body and the choroid. Inflammation of any of these parts is termed uveitis.
Based on the part of the uvea involved, uveitis may be Anterior (involving the iris), Intermediate (involving the ciliary body), Posterior (involving the choroid) or Panuveitis (involving all the parts).
Symptoms of uveitis are highly variable and may include any of the following: redness, pain, watering, inability to see bright light, floaters, and / or decreased vision.
Uveitis occurs as a result of an immune reaction by our body to antigens (substances our body considers foreign). This reaction may occur against infectious agents such as bacteria, fungi, viruses and even parasites. In a small subset of patients, uveitis can occur due to undeterminable causes.
Uveitic patients often require a whole battery of investigations in order that the underlying cause of uveitis be determined and hence appropriately treated. These usually include blood and urine tests and/ or X rays. At times, a sample of the fluid from the patients’ eye may have to be subjected to lab tests.
Steroids are the mainstay of treatment in uveitis. Depending on the location and the severity of the inflammation, they are used in the form of eye drops, , injections around/ in the eye or injectable / oral medications. Anterior (and intermediate) uveitis is treated with topical steroids along with dilating eye drops which help in reducing the pain associated with inflammation. These drops are to be used until the inflammation has completely subsided. The dose, strength and duration of the drops are determined by your doctor who decides the treatment in accordance to the amount of inflammation.
Injection of the steroid around the eye (periocular steroids) is used in certain cases of intermediate uveitis (or in macular edema as a consequence of uveitis). This results in slow release of the drug over a period of three to four weeks.
Injectable/oral steroids are often indicated in posterior/panuveitis.
Besides steroids, the other group of drugs used in the treatment of uveitis is immunosuppressives. These are especially reserved for patients intolerant to steroids, inflammation not resolving with only steroids and patients with certain systemic conditions like rheumatoid arthritis
Both steroids and immunosuppressives have side effects that are often not serious and reversible following the discontinuation of the drugs. These drugs should always be taken as per your doctors’ instructions. Never start or stop these drugs of you own accord. It is important to remember that uveitis is a recurrent condition and hence requires a prolonged and regular follow up with your doctor. Consult your ophthalmologist at the earliest signs of a recurrence. This will make treatment easier and resolution speedier.
Uveitic patients may develop cataract (opacification of the lens), glaucoma (raised intraocular pressure) and macular edema (swelling of the central part of the retina) in addition to the inflammation itself. These complications may require additional medical or surgical management.


